Clinical Tips: Periodontal Microscopy and Endoscopy – RDHmag.com
Welcome to an insightful guide exploring periodontal microscopy and endoscopy, two cutting-edge diagnostic and treatment aids reshaping modern dental hygiene and periodontology. As highlighted by experts on RDHmag.com, these technologies provide unprecedented visualization of periodontal structures, allowing clinicians to elevate patient care dramatically. Whether you’re a dental hygienist, periodontist, or clinical specialist, this article offers practical clinical tips, benefits, and real-world applications to maximize the value of periodontal microscopy and endoscopy in your practice.
Understanding Periodontal Microscopy and Endoscopy
Before diving into tips and benefits, it’s essential to understand what periodontal microscopy and endoscopy entail:
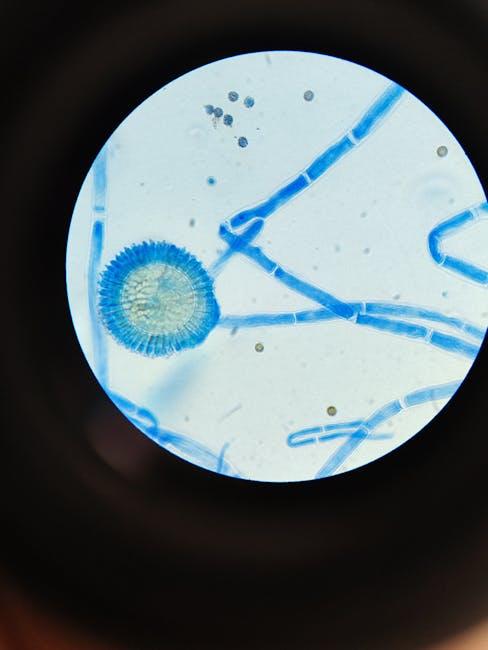
- Periodontal Microscopy: Utilizes magnification devices such as dental operating microscopes or loupes with high magnification to visualize gingival and subgingival structures during periodontal therapy.
- Periodontal Endoscopy: Involves the use of miniature fiber-optic cameras inserted into periodontal pockets to provide high-resolution, real-time imaging of hard-to-see root surfaces, deposits, and tissue conditions.
Both technologies provide enhanced precision during procedures like scaling, root planing, and surgical interventions.
Why Integrate Periodontal Microscopy and Endoscopy into Your Practice?
| Benefits | Description |
|---|---|
| Improved Visualization | Clearly view calculus, biofilm, and root morphology below the gumline. |
| Enhanced Treatment Accuracy | Precisely remove deposits and avoid damage to delicate tissues. |
| Early Disease Detection | Identify pockets, inflammation, or root defects earlier for timely intervention. |
| Patient Education | Show patients intraoral images to increase treatment acceptance and compliance. |
| Better Outcomes | Increase success rates of nonsurgical and surgical periodontal therapy. |
Clinical Tips for Using Periodontal Microscopy
Using periodontal microscopes effectively requires some essential clinical approaches to maximize their benefits and make procedures more efficient:
1. Start With Proper Magnification Selection
Choose an appropriate magnification level, typically between 4x and 25x, based on the clinical task. Lower magnification suits general visualization, while higher magnification helps in detecting microscopic calculus and fine details.
2. Optimize Lighting and Ergonomics
Ensure a shadow-free light source integrated with the microscope to illuminate subgingival sites clearly. Maintain proper posture and positioning to avoid operator fatigue and ensure precise hand movements.
3. Integrate Microscopy Into Every Periodontal Procedure
Incorporate microscopy during scaling, root planing, and microsurgical techniques. This will minimize the risk of incomplete calculus removal and reduce the need for retreatments.
4. Enhance Patient Communication
Use microscope camera outputs or capture images to explain findings to patients. Visualization builds trust and helps patients understand the importance of periodontal care.
Practical Tips for Periodontal Endoscopy Deployment
Periodontal endoscopy is a sophisticated tool—setup and technique matter a lot. Consider these tips:
- Master Proper Insertion: Gently introduce the endoscope into periodontal pockets to avoid tissue trauma. Use lubrication if necessary.
- Maintain Clear Visual Fields: Regularly irrigate pockets during endoscopy to flush blood and debris from the camera lens.
- Document Findings: Capture high-quality images or video segments for records and case presentations.
- Use Endoscopy to Target Calculus: Visualize hidden subgingival deposits precisely and confirm their complete removal.
- Continuously Update Skills: Attend manufacturer workshops and online training to stay current with evolving techniques.
Case Study: Enhanced Nonsurgical Treatment Using Periodontal Endoscopy
Patient Profile: 48-year-old male with moderate chronic periodontitis, pocket depths ranging from 5mm to 7mm.
Approach:
- Initial periodontal assessment with traditional probing and radiographs.
- Use of periodontal endoscopy for subgingival visualization prior to scaling.
- Targeted removal of localized calculus confirmed via endoscopic imaging.
- Post-procedure evaluation showed significantly cleaner root surfaces compared to standard techniques.
Outcome: Follow-up at 3 months revealed decreased pocket depths and improved clinical attachment levels, with higher patient satisfaction due to less postoperative discomfort.
First-Hand Experience: RDH’s Perspective on Microscopy and Endoscopy
Dental hygienists often find periodontal microscopy and endoscopy to be game-changers in their clinical routine. An experienced RDH comments:
“Incorporating microscopy into my daily practice has revolutionized how I perform deep cleanings. It’s like turning on a light in a dark room—I can see the tiniest deposits and address them immediately. Endoscopy adds another layer of confidence because I can visually confirm calculus removal without guessing. My patients appreciate the visual education and improved results.”
More Tips to Maximize Success With These Technologies
- Regular Equipment Maintenance: Keep lenses, fiber optics, and sensors clean for optimal image clarity.
- Patient Preparation: Explain procedures beforehand to ease patient anxiety about new technology.
- Team Training: Involve the entire dental team in training sessions to streamline workflow.
- Documentation: Use images and videos from microscopy and endoscopy for insurance and treatment planning.
Common Challenges and How to Overcome Them
| Challenge | Solution |
|---|---|
| Fogging of the Endoscope Lens | Pre-warm the scope and use anti-fog solutions before insertion. |
| Limited Pocket Access | Use smaller diameter scopes or micro-instruments designed for tight spaces. |
| Operator Fatigue | Take regular breaks and adjust ergonomic setup including chair height and scope positioning. |
| Patient Discomfort | Apply topical anesthetics and use gentle insertion and movement techniques. |
Conclusion
Periodontal microscopy and endoscopy, championed by leading voices at RDHmag.com, represent transformative advancements in periodontal care. By enhancing visualization and precision, these tools empower clinicians to deliver superior treatment outcomes and elevate patient experiences. Integrating these technologies into your practice may require an initial learning curve and investment, but the clinical benefits — improved accuracy, early detection, and enhanced patient education — make it a worthwhile evolution in dental hygiene and periodontology. Use the clinical tips and strategies provided to optimize your use of periodontal microscopy and endoscopy and stay at the forefront of minimally invasive, high-quality periodontal therapy.