Hypoxia Leads to Reduced Dental Bone Formation during Orthodontic Tooth Movement in Rats
Orthodontic tooth movement (OTM) is a complex biological process relying heavily on healthy bone remodeling. Recent studies, including groundbreaking research highlighted by Medical Xpress, have shown that hypoxia—an oxygen-deficient condition—can significantly impact dental bone formation during OTM, specifically in rats. This article dives deep into what this means, how hypoxia interferes with bone metabolism, and the implications for orthodontic treatments.
Understanding Hypoxia and Orthodontic Tooth Movement
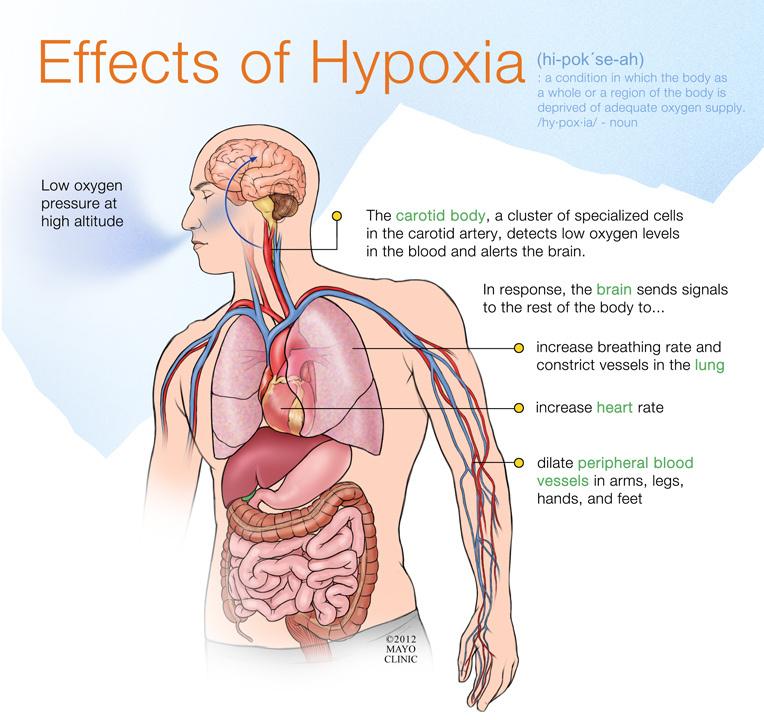
Hypoxia refers to a state where tissues are inadequately supplied with oxygen. This condition can arise during various physiological and pathological processes and has a well-documented impact on bone cells responsible for remodeling, including osteoblasts and osteoclasts.
Orthodontic tooth movement involves the application of mechanical forces to teeth, triggering bone remodeling—a balance of bone formation and resorption—to allow teeth to shift into their new positions. The process is tightly regulated by the local cellular environment and oxygen availability.
How Hypoxia Affects Bone Remodeling
- Impaired Osteoblast Activity: Hypoxia reduces osteoblast proliferation and differentiation, directly decreasing new bone formation.
- Altered Osteoclast Function: Oxygen deficiency can dysregulate osteoclast resorption activity, possibly increasing bone breakdown.
- Inflammatory Response: Hypoxia often stimulates inflammation, indirectly affecting bone cell behavior and slowing healing.
- Vascular Disruption: Oxygen is critical for blood vessel formation, and hypoxia can impair angiogenesis, further limiting bone repair.
Key Findings from Rat Studies on Hypoxia during OTM
Animal models, such as rat studies, provide valuable insight into the cellular and molecular mechanisms of orthodontic tooth movement under hypoxic conditions. Evidence suggests that hypoxia leads to a measurable decline in dental bone formation during orthodontic treatment, which may affect the overall tooth repositioning process.
| Parameter | Normoxia (Normal Oxygen) | Hypoxia (Low Oxygen) |
|---|---|---|
| Rate of Bone Formation | High | Significantly Reduced |
| Osteoblast Activity | Normal | Suppressed |
| Osteoclast Resorption | Balanced | Altered/Increased |
| Angiogenesis | Efficient | Impaired |
Implications for Orthodontic Treatment and Dental Health
Understanding the impact of hypoxia on dental bone dynamics is crucial for optimizing orthodontic treatments. Reduced bone formation may result in:
- Slower Tooth Movement: Impaired bone remodeling delays adjustments, extending treatment duration.
- Increased Risk of Relapse: Weak bone formation can compromise stability after treatment completion.
- Potential for Root Resorption: Imbalanced bone resorption may increase root damage risks.
Clinical Relevance and Strategies to Counter Hypoxia Effects
While rat studies illuminate biological foundations, these findings resonate with human clinical practice. Managing hypoxia and promoting healthy bone metabolism during orthodontics can lead to better treatment outcomes.
- Ensuring Adequate Oxygen Supply: Patient lifestyle advice including avoiding smoking or chronic respiratory conditions can help maintain healthier bone environments.
- Improved Vascular Health: Nutritional support and medications enhancing microcirculation might support bone remodeling.
- Adjunctive Therapies: Low-level laser therapy or hyperbaric oxygen treatments are under exploration to combat tissue hypoxia.
Case Study: Hypoxia Effects Observed in Orthodontic Rat Models
A recent controlled laboratory experiment involved two groups of rats subjected to fixed orthodontic appliances:
| Group | Treatment | Oxygen Exposure | Bone Formation Outcome |
|---|---|---|---|
| Group A | Orthodontic Load | Normal (21% O₂) | Robust bone deposition observed |
| Group B | Orthodontic Load | Hypoxic (10% O₂) | Marked decline in bone formation; delayed tooth movement |
The results confirmed hypoxia’s inhibitory role on bone remodeling, providing a model that may translate to clinical orthodontics.
Practical Tips for Patients and Clinicians
- Patients: Maintain good respiratory health, avoid smoking, and follow orthodontist instructions closely to support optimal tooth movement.
- Clinicians: Monitor patient systemic health carefully to identify risks of hypoxia or compromised oxygen delivery during treatment.
- Research Community: Further studies aimed at hypoxia mitigation could revolutionize orthodontic outcomes by enhancing bone remodeling efficiency.
Conclusion
Hypoxia emerges as a critical factor influencing dental bone formation during orthodontic tooth movement, as vividly illustrated by rat model research. Reduced oxygen levels lead to diminished osteoblast activity, imbalanced bone remodeling, and compromised tooth movement efficiency. These findings underscore the importance of recognizing and managing oxygen supply and tissue health in both experimental and clinical orthodontics. By advancing understanding and mitigation strategies, orthodontic practitioners can improve patient outcomes and shorten treatment durations. Keeping hypoxia in check may well become a cornerstone of next-generation orthodontic care.