Insights Into the Role of Streptococcus mutans and Candida albicans in Dental Biofilm Formation and Cariogenicity: A Literature Review – Cureus
Dental caries remains one of the most prevalent chronic diseases worldwide, primarily attributed to complex microbial interactions within dental biofilms. Among the multifaceted microbiota, Streptococcus mutans and Candida albicans have gained significant attention due to their synergistic role in dental biofilm formation and cariogenicity. This literature review highlights recent scientific insights into how these two microorganisms contribute to oral disease progression, emphasizing their interaction, mechanisms, and implications for prevention and treatment.
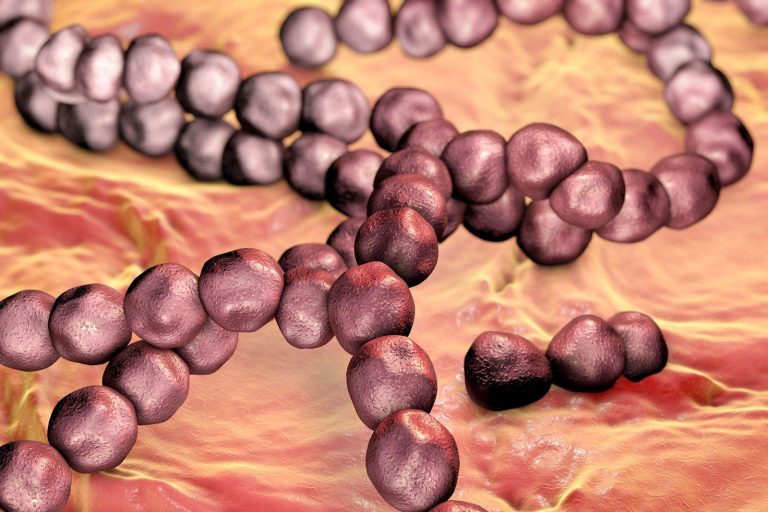
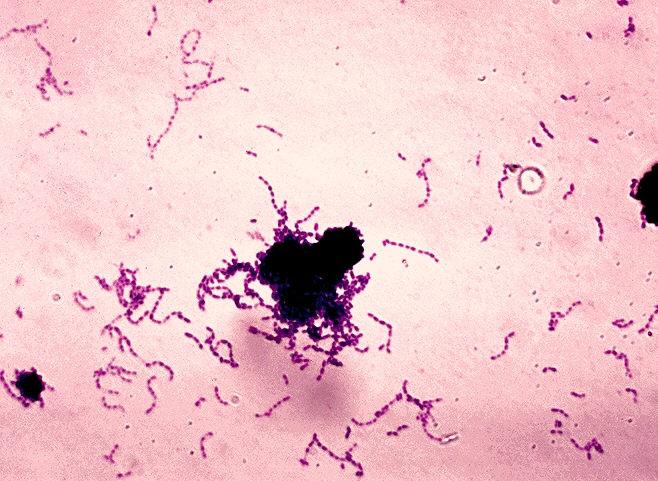
The Basics: What Are Streptococcus mutans and Candida albicans?
Streptococcus mutans is a gram-positive, facultative anaerobic bacterium that plays a pivotal role in the initiation and development of dental caries through acidogenic and aciduric properties. It metabolizes dietary sugars to produce lactic acid, which demineralizes tooth enamel, leading to cavity formation.
Candida albicans, on the other hand, is a common fungal inhabitant of the oral cavity. While typically a commensal organism, under dysbiotic conditions, it can contribute to oral infections like candidiasis. Emerging studies suggest C. albicans also participates actively in dental biofilm maturation and enhances cariogenic potential when coexisting with S. mutans.
Understanding Dental Biofilms and Their Cariogenicity
Dental biofilms are intricate microbial communities embedded in a matrix of extracellular polymeric substances (EPS), firmly adhering to tooth surfaces. The cariogenic potential depends largely on the biofilm’s composition, structure, and metabolic activities.
- Biofilm formation stages: initial adhesion, microcolony formation, maturation, and dispersal.
- Role of EPS: provides structural stability and protection, facilitating microbial communication and resistance.
- Acid production: leads to enamel demineralization when acidogenic microbes dominate.
The Synergistic Interaction Between S. mutans and C. albicans
Recent literature reveals a dynamic and mutually enhancing relationship between these two species within cariogenic biofilms:
- Enhanced adhesion: S. mutans produces glucosyltransferase (GtfB) enzymes that bind to C. albicans surfaces, increasing fungal attachment to tooth enamel.
- Biofilm biomass increment: Co-culture biofilms exhibit thicker, more robust structures compared to mono-species biofilms, favoring persistence and virulence.
- Increased acidogenicity: Metabolic interactions promote acid production, accelerating enamel demineralization.
- Resistance to host defense: Dual-species biofilms show enhanced resistance to antimicrobial agents and host immune responses.
Table: Key Differences Between Mono-Species and Dual-Species Biofilms
| Feature | S. mutans Only | S. mutans + C. albicans |
|---|---|---|
| Biofilm Thickness | Moderate | Significantly Increased |
| Acid Production | High | Very High |
| Resistance to Antimicrobials | Moderate | Enhanced |
| Adhesion to Tooth Surface | Strong | Stronger |
Mechanisms of Cariogenicity in Dual-Species Biofilms
The cariogenicity of S. mutans and C. albicans biofilms is attributed to several factors:
- Glucosyltransferase activity: GtfB binds to C. albicans, synthesizing glucans that enhance fungal incorporation into biofilms.
- Extracellular matrix development: The combined EPS generated strengthens the biofilm’s architecture, providing a protective niche.
- Acid tolerance: C. albicans contributes to the acidic microenvironment by surviving low pH and fostering S. mutans growth.
- Metabolic synergy: Metabolic cross-feeding helps sustain prolonged acid production and biofilm stability.
Clinical Implications and Risk Factors
The interplay of S. mutans and C. albicans influences the severity and progression of dental caries, especially in susceptible populations such as children, immunocompromised individuals, and those with poor oral hygiene.
Contributing risk factors include:
- High sugar intake supplying substrate for acidogenic microbes.
- Reduced salivary flow impairing natural biofilm clearance.
- Frequent antibiotic or corticosteroid use altering oral microbial balance.
- Poor oral hygiene promoting microbial accumulation.
Preventive Tips and Practical Recommendations
Understanding the dual role of S. mutans and C. albicans provides opportunities for targeted prevention strategies against dental caries.
- Maintain thorough oral hygiene: Brushing twice daily with fluoride toothpaste and flossing to disrupt biofilms.
- Limit dietary sugars: Reducing fermentable carbohydrate intake to starve cariogenic microbes.
- Use antimicrobial agents: Chlorhexidine or antifungal rinses in at-risk patients under professional guidance.
- Regular dental visits: Professional plaque removal and assessment for early caries management.
- Salivary flow support: Stay hydrated and use saliva substitutes if necessary.
Emerging Research and Future Directions
Cutting-edge studies are exploring novel therapeutic targets, including disrupting the binding of GtfB to C. albicans or interfering with biofilm EPS synthesis to weaken biofilm formation.
Probiotics and natural antimicrobial compounds are being investigated as adjunctive therapies to modulate oral microbiota composition favorably.
Conclusion
The synergistic relationship between Streptococcus mutans and Candida albicans plays a crucial role in dental biofilm development and heightened cariogenicity. Their interaction amplifies biofilm virulence, acid production, and resistance to treatment, deepening our understanding of cariogenesis beyond simple bacterial involvement. Incorporating this knowledge into clinical practice empowers better-targeted preventive measures, improved diagnostic approaches, and innovative therapeutics that could revolutionize oral health care.
Ongoing research continues to unravel the complex molecular dynamics of these dual-species biofilms, holding promise to mitigate the global burden of dental caries effectively.