Ottawa Is Underfunding Pharmacare and Dental Care, Exacerbating Current Inequities: Nigel Rawson and John Adams — A National Post Spotlight via The Macdonald-Laurier Institute
Canada is renowned for its universal healthcare system, but significant cracks remain beneath the surface — especially in pharmacare and dental care coverage. In a compelling National Post piece by Nigel Rawson and John Adams, representing the expertise of the Macdonald-Laurier Institute, concerns have been raised about Ottawa’s chronic underfunding in these critical healthcare sectors. Their analysis argues this funding gap worsens existing health inequities across Canadian communities.
Understanding the Current State: Pharmacare and Dental Care in Canada
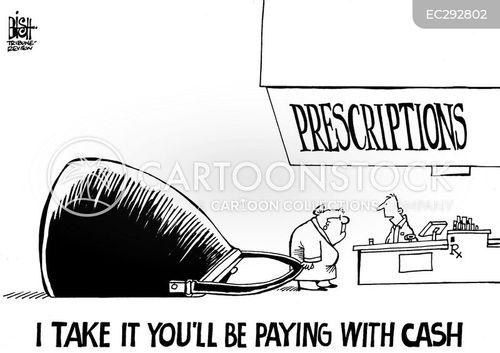
While Canada’s public health insurance covers hospital and physician services, prescription drugs and dental care are often left to patchwork provincial programs, private insurance, or out-of-pocket payments. This disparity creates uneven access, leading to poorer health outcomes for marginalized populations.
Pharmacare Funding: What’s Missing?
Canada’s lack of a comprehensive, universally accessible pharmacare program means many citizens can’t adequately afford their medications. Ottawa’s funding has historically been insufficient, contributing to:
- High prescription drug costs for uninsured or underinsured Canadians
- Disparities in medication adherence and health outcomes
- Increased financial strain on low-income families
Dental Care: The Forgotten Essential
Contrary to popular belief, dental care is not universally covered in Canada. This leaves millions vulnerable, particularly those with low incomes or living in rural areas. The consequences include:
- Delayed preventative dental visits leading to worsening oral health
- Higher incidence of costly emergencies and systemic health complications
- Exacerbation of socio-economic health inequities
Insights from Nigel Rawson and John Adams: The Core Arguments
Rawson and Adams emphasize that underfunding pharmacare and dental care is not merely a budget oversight — it’s an issue with deep social and economic repercussions. Below are key takeaways from their analysis:
- Underinvestment fuels inequity: Without adequate funding, marginalized groups bear disproportionate health burdens.
- Comprehensive coverage reduces costs long-term: Investing in pharmacare and dental care upfront reduces hospital admissions and chronic disease progression.
- Multi-level collaboration is essential: Coordinated federal-provincial efforts must bridge current coverage gaps.
- Evidence-based policy-making: Policy must be informed by robust data highlighting coverage shortfalls and health outcomes.
The Health Equity Gap: How Underfunding Deepens Disparities
Health inequities in Canada often correlate strongly with socio-economic status, geography, and age groups. Ottawa’s funding gaps disproportionately affect:
- Low-income families unable to afford private insurance
- Elderly Canadians on fixed incomes
- Indigenous communities with limited access to services
- Rural residents with fewer healthcare providers
Below is a simple overview of how underfunding impacts these groups:
| Group | Pharmacare Impact | Dental Care Impact |
|---|---|---|
| Low-income Families | Unable to afford essential meds; increased hospital visits | Dental problems untreated; emergency care more frequent |
| Elderly | Polypharmacy risks; medication non-adherence | Higher risk of oral infections affecting general health |
| Indigenous Communities | Limited coverage leads to untreated chronic illness | Dental access barriers; higher oral disease rates |
| Rural Residents | Scarce pharmacies; high drug costs | Few dentists; travel required for treatment |
Benefits of Investing in Pharmacare and Dental Care
The Macdonald-Laurier Institute highlights multiple benefits if Ottawa increases funding and implements universal coverage initiatives:
- Improved population health: Better medication adherence and oral hygiene reduce chronic disease risks.
- Cost savings: Preventative care reduces emergency department visits and hospital stays.
- Greater social equity: Accessible care levels the healthcare playing field for vulnerable Canadians.
- Economic productivity: Healthier Canadians contribute more effectively to the economy.
Practical Recommendations for Addressing Funding Gaps
Rawson and Adams suggest actionable strategies for policymakers and stakeholders to begin bridging these critical gaps in pharmacare and dental care:
- Federal-Provincial Collaboration: Harmonize funding frameworks ensuring comprehensive coverage across jurisdictions.
- Incremental Implementation: Start with essential drug lists and core dental services before expanding universally.
- Target Vulnerable Populations: Prioritize low-income groups, seniors, and Indigenous peoples in program rollouts.
- Public Awareness Campaigns: Educate Canadians on benefits and availability of pharmacare and dental care programs.
- Data-Driven Policy: Use measurable outcomes to guide future funding adjustments and program scaling.
Case Study: Provincial Pharmacare Innovation in British Columbia
British Columbia’s recent expansion of pharmacare coverage provides a real-world example demonstrating the benefits of increased funding and broader access. Key results include:
- Significant reductions in out-of-pocket drug costs for residents
- Improved medication adherence for chronic disease patients
- Lower hospitalization rates related to medication non-compliance
This success story offers a blueprint Ottawa could apply nationwide to reduce inequities stemming from underfunding.
Conclusion: Closing the Gap for a Healthier, More Equitable Canada
Nigel Rawson and John Adams’ insightful critique in The National Post reveals an urgent truth: Ottawa’s inadequate funding for pharmacare and dental care is deepening health inequities rather than alleviating them. With millions affected — especially marginalized Canadians — the need for a strategic, well-funded, and inclusive policy approach has never been greater.
By embracing comprehensive pharmacare and dental care coverage, supported by sustained federal investments and coordinated provincial action, Canada can move closer to truly universal healthcare. Doing so will create better health outcomes, reduce healthcare costs in the long run, and promote fairness across Canadian society.
If Canada is to maintain its reputation as a leader in healthcare accessibility, the time for change is now — and Ottawa’s funding decisions will determine the health and wellbeing of generations to come.