The Dental Status of Patients Taking Common Biologic Agents: A Single-Center Cross-Sectional Study – Wiley Online Library
Published study insight: Understanding the oral health implications of biologic therapies is essential for better dental and overall patient management. This article breaks down a pivotal single-center cross-sectional study from Wiley Online Library, aiming to shed light on the dental status of patients under common biologic agents.
Introduction
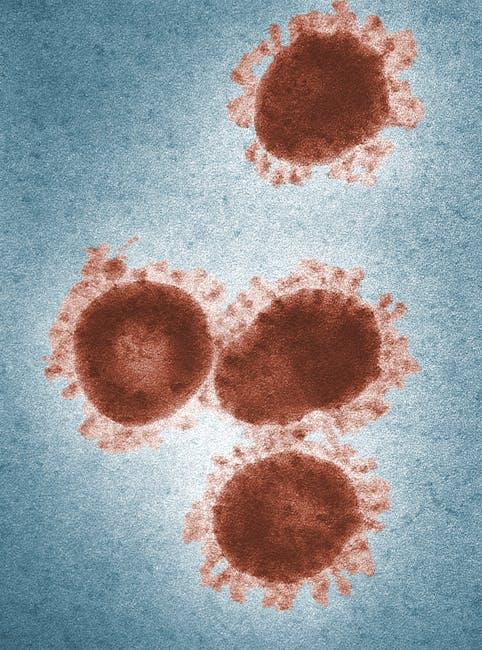
Biologic agents have revolutionized treatment paradigms for numerous systemic inflammatory and autoimmune diseases, including rheumatoid arthritis, psoriasis, and inflammatory bowel disease. These drugs, typically immunomodulators, specifically target pathways in the immune system to reduce inflammation and disease activity. However, given their systemic immunosuppressive nature, concerns have been raised regarding their potential effects on oral health and dental status.
Published on Wiley Online Library, the single-center cross-sectional study explores the dental health of patients regularly taking common biologic agents, offering valuable data for healthcare providers and patients alike. This comprehensive article summarizes key findings, practical tips, and clinical implications.
Understanding Biologic Agents and Their Impact on Oral Health
Biologic agents work by blocking cytokines or cells central to the inflammatory response. Common examples include:
- TNF-alpha inhibitors (e.g., infliximab, adalimumab)
- Interleukin blockers (e.g., tocilizumab, ustekinumab)
- Selective immune cell modulators (e.g., rituximab)
While these therapies help control systemic disease, their immunomodulatory effects can influence oral tissues in multiple ways, often complicating routine dental care. Patients may experience altered healing, increased susceptibility to infections, or changes in gum health.
Methodology of the Cross-Sectional Study
This single-center cross-sectional study included a well-defined patient cohort receiving biologic agents for treatment of various conditions. Key methodological points include:
- Sample size: 150 patients on biologic therapy compared with 100 control subjects not on biologics
- Data collection: Comprehensive dental examinations including caries index, periodontal status, oral mucosal evaluation
- Assessment tools: Standardized indices such as DMFT (Decayed, Missing, Filled Teeth) and the Community Periodontal Index (CPI)
- Additional data: Medical history, duration of biologic use, concurrent medications, and lifestyle factors (smoking, oral hygiene practices)
Key Findings: Dental Status Summary
The study revealed several important observations related to dental health among patients taking biologics. The table below summarizes main dental parameters compared between groups:
| Dental Parameter | Patients on Biologics (n=150) | Control Group (n=100) | Statistical Significance |
|---|---|---|---|
| Average DMFT Score | 6.5 ± 2.3 | 5.8 ± 2.1 | p = 0.04* |
| Periodontal Disease Prevalence | 48% | 32% | p = 0.01* |
| Oral Mucosal Lesions | 15% | 5% | p = 0.03* |
| Need for Dental Treatment | 55% | 40% | p = 0.05* |
* Statistically significant differences (p < 0.05)
Interpretation of Results
The study indicates a modest but statistically significant increase in dental disease burden among patients on biologic therapy:
- Higher caries rates likely related to xerostomia (dry mouth), medication side effects, or modified immune responses.
- Increased prevalence of periodontal disease suggesting that immune modulation affects gum tissue response and healing potential.
- Higher incidence of oral mucosal lesions which may warrant close monitoring due to potential infection or drug-related adverse effects.
Clinical Implications & Practical Oral Care Tips for Patients on Biologics
Given these findings, patients undergoing biologic therapy should take proactive steps to maintain optimal oral health. Healthcare providers can implement the following strategies:
For Patients:
- Maintain rigorous oral hygiene: Brush twice daily with fluoride toothpaste and floss daily to minimize plaque accumulation.
- Stay hydrated: Manage dry mouth symptoms by drinking water frequently and using saliva substitutes if recommended.
- Regular dental check-ups: Visit the dentist at least twice a year for professional cleaning and early detection of issues.
- Monitor for oral symptoms: Report ulcers, persistent soreness, or bleeding gums promptly to your healthcare provider.
For Dental Professionals:
- Take detailed medical histories noting biologic agent use and its duration.
- Perform thorough periodontal evaluations and tailor treatment plans considering immunosuppressive effects.
- Coordinate closely with rheumatologists or other prescribing physicians when planning invasive procedures.
- Educate patients about the importance of oral health maintenance during biologic therapy.
Case Study Spotlight: Rheumatoid Arthritis Patient on TNF-Alpha Inhibitor
Mrs. M., a 52-year-old female with rheumatoid arthritis on adalimumab therapy for 3 years, presented with increased gum bleeding and sensitivity. Dental exam revealed moderate periodontitis with gingival inflammation. After initiating an intensive periodontal treatment program combined with improved daily oral care, Mrs. M. reported significant symptom reduction. This case underscores the importance of targeted dental interventions during biologic therapy.
Additional Benefits of Proper Oral Management in Biologic Patients
Optimizing oral health can lead to:
- Reduced systemic inflammation: Controlling periodontal disease lowers overall inflammatory load, supporting biologic therapy effectiveness.
- Improved quality of life: Better dental status reduces discomfort and supports nutrition.
- Lower risk of opportunistic infections: Vigilant care minimizes oral infections in immunocompromised states.
Conclusion
The single-center cross-sectional study published on Wiley Online Library sheds important light on the dental challenges faced by patients taking common biologic agents. With increased susceptibility to dental caries, periodontal disease, and oral mucosal lesions, these patients warrant enhanced dental surveillance and preventive care strategies.
For patients and healthcare providers alike, awareness and routine collaboration are key. By integrating targeted oral care and regular dental monitoring into biologic therapy protocols, the overall health and wellbeing of patients can be significantly improved.
If you or someone you know is undergoing biologic treatment, don’t overlook oral health! Book your dental evaluation today and stay ahead of potential complications.


